Pathological non-response to chemotherapy in a neoadjuvant setting of breast cancer: an inter-institutional study
Balmativola, D., C. Marchio, M. Maule, L. Chiusa, L. Annaratone, F. Maletta, F. Montemurro, J. Kulka, P. Figueiredo, Z. Varga, I. Liepniece-Karele, G. Cserni, E. Arkoumani, I. Amendoeira, G. Callagy, A. Reiner-Concin, A. Cordoba, S. Bianchi, T. Decker, D. Glaser, C. Focke, P. van Diest, D. Grabau, E. Lips, J. Wesseling, R. Arisio, E. Medico, C. Wells and A. Sapino (2014).
Breast Cancer Res Treat 148(3): 511-523.
http://www.ncbi.nlm.nih.gov/pubmed/25395316
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4243004/pdf/10549_2014_Article_3192.pdf
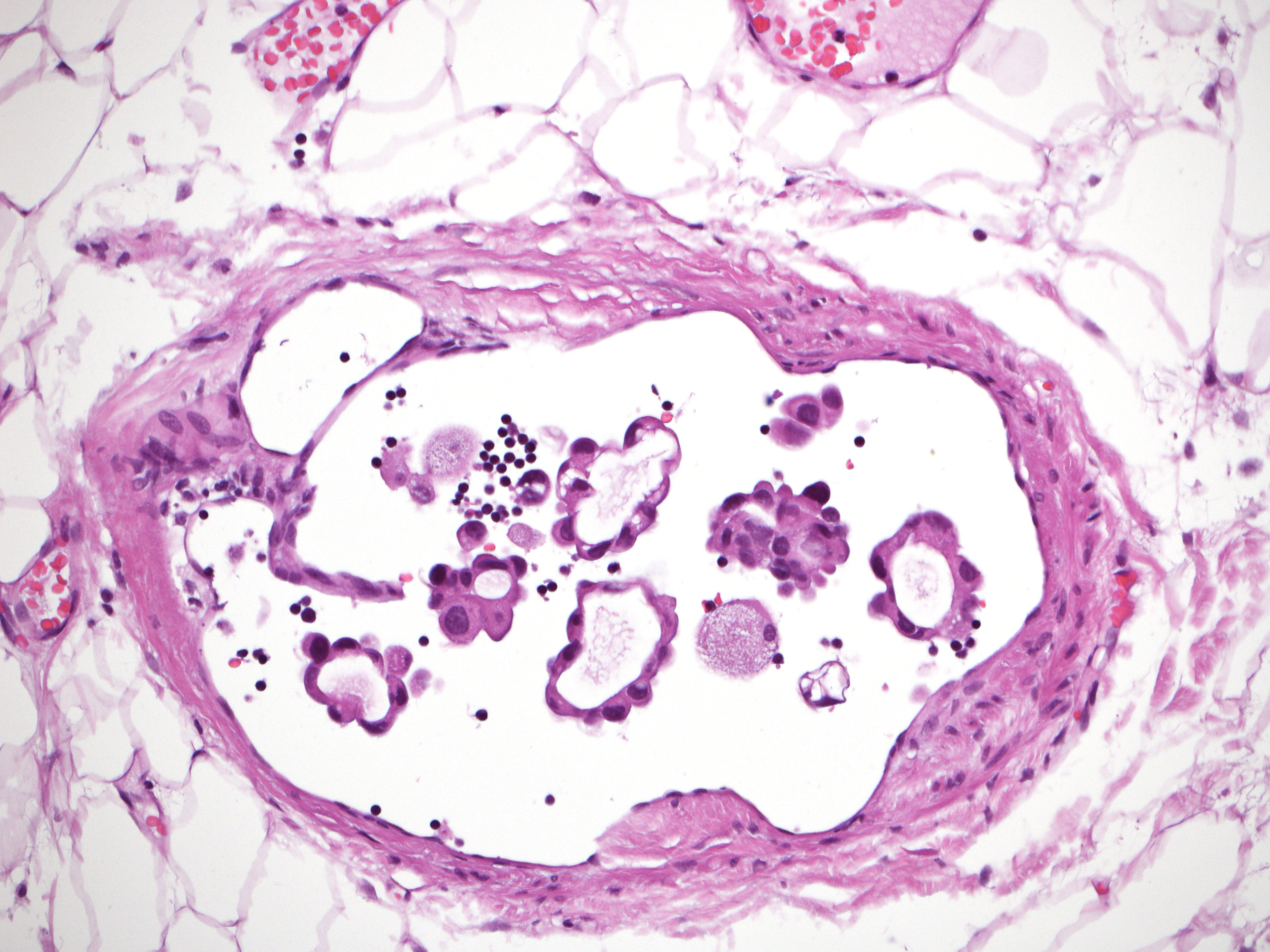
To identify markers of non-response to neoadjuvant chemotherapy (NAC) that could be used in the adjuvant setting. Sixteen pathologists of the European Working Group for Breast Screening Pathology reviewed the core biopsies of breast cancers treated with NAC and recorded the clinico-pathological findings (histological type and grade; estrogen, progesterone receptors, and HER2 status; Ki67; mitotic count; tumor-infiltrating lymphocytes; necrosis) and data regarding the pathological response in corresponding surgical resection specimens. Analyses were carried out in a cohort of 490 cases by comparing the groups of patients showing pathological complete response (pCR) and partial response (pPR) with the group of non-responders (pathological non-response: pNR). Among other parameters, the lobular histotype and the absence of inflammation were significantly more common in pNR (p < 0.001). By ROC curve analyses, cut-off values of 9 mitosis/2 mm(2) and 18% of Ki67-positive cells best discriminated the pNR and pCR + pPR categories (p = 0.018 and < 0.001, respectively). By multivariable analysis, only the cut-off value of 9 mitosis discriminated the different response categories (p = 0.036) in the entire cohort. In the Luminal B/HER2- subgroup, a mitotic count <9, although not statistically significant, showed an OR of 2.7 of pNR. A lobular histotype and the absence of inflammation were independent predictors of pNR (p = 0.024 and <0.001, respectively). Classical morphological parameters, such as lobular histotype and inflammation, confirmed their predictive value in response to NAC, particularly in the Luminal B/HER2- subgroup, which is a challenging breast cancer subtype from a therapeutic point of view. Mitotic count could represent an additional marker but has a poor positive predictive value.